From the desk of: Jomari Torres, M.D.
Obesity is a disease that impacts all levels of society. It is the most prevalent nutritional disorder among children and adolescents and is continuing to rise. In 2012 more than one-third of children and adolescents were overweight or obese. According to the Centers for Disease Control and Prevention (CDC), childhood obesity has more than doubled in children and quadrupled in adolescents over the past 30 years.
Why is being overweight or obese such an issue?
Obesity is considered a major health concern in developed countries: overweight children are at higher risk of becoming overweight adolescents, and overweight adolescents are at higher risk of becoming overweight adults. The younger the age of the child when he or she becomes overweight the higher the risk for future obesity.
Although children have, in general, fewer health-related problems associated with being overweight, we are starting to see more overweight and obese children develop problems with:
- High blood pressure
- High cholesterol
- Heart disease at a young age
- Diabetes
- Sleep apnea
- Cancer (including breast, colon, esophagus, kidney, pancreas, thyroid, ovary, prostate, multiple myeloma and Hodgkin’s lymphoma)
- Low self-esteem and depression due to social discrimination
Causes of childhood obesity
Children become overweight and obese for a variety of reasons, including genetics, physical and social environment (access to healthy and affordable food, exposure to advertisements for junk foods, lack of safe areas to exercise, lack of walkable neighborhoods) and lifestyle or behaviors (choices in diet and level of physical activity). However, less than 10% of all the cases are associated with hormonal or genetic causes. Therefore, the majority of cases are due to environment and behaviors, making intervention in these areas a promising treatment or cure for this disease.
How do I know if my child is overweight or obese?
Most healthcare providers define childhood obesity by using the Body Mass Index (BMI). BMI is an estimate of body fat that uses weight and height for its calculation. Because children change rapidly as they grow, age and sex of the child are also used in BMI calculations. A child with a BMI greater than the 95th percentile by age is considered obese, and a child with a BMI between 85th and 95th percentile by age is considered overweight. Healthy BMI for age percentiles for children is between 5% and 85%. It should be kept in mind that BMI is a method to help in the assessment of body fat and only a physician can best determine and diagnose your child as overweight or obese.
What can we do as a parent, a family member, and a friend, to help control this disease affecting our children?
Because this disease is multifactorial in origin, the approach must be the same.
Environment – While it is not always possible to change where we live, we can limit some negative influences on our children and increase positive ones.
- Today children spend many hours watching television, playing video games or online. As a result they not only spend less time being active, they also are exposed to commercials promoting unhealthy foods and eating habits. Half of all commercials are about the fast food industry.
- Restrict screen time for children and encourage active time.
- Make it a priority to teach children that food is a nutrient and energy source for our bodies and not a comfort. Teach by example by making your own healthy food choices for meals and snacks.
- Many children lack enough physical activity. Due to our busy schedules with work and school, fewer families are involved in outside activities on a regular basis. Children depend more on electronic media to complete homework taking away the time they spend being active
- Take 30 minutes twice a day to jump or dance with your kids. Be silly with them. Show them that being active is fun and not another chore. It is a break time, and they will learn to cherish activity.
Diet – Learn about the government’s new dietary guidelines, which emphasize eating whole grains, fruits, vegetables, lean protein, low-fat and fat-free dairy products and drinking water, while limiting saturated and trans fats, added sugars, and sodium.
- More families rely on restaurants, fast foods and cafeterias for daily meals.
- Be aware of added sugars, sodium and “bad” fats in restaurant foods and try to make choices that would limit these.
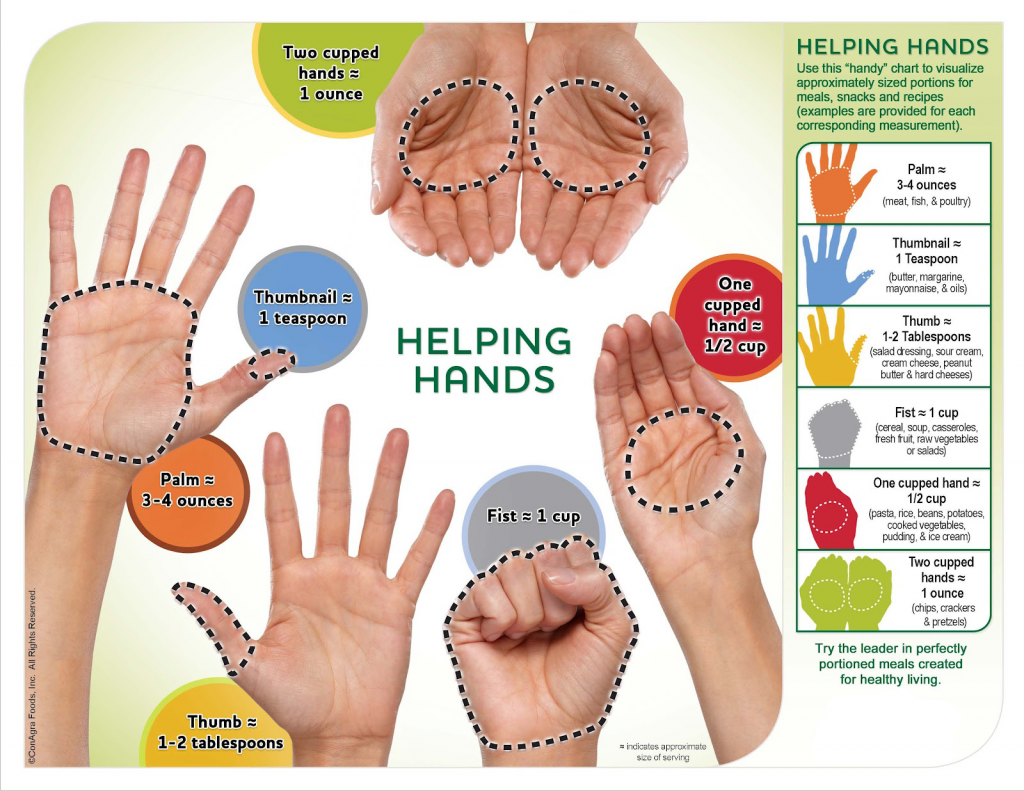
- Portion size and caloric intake have increased dramatically. Think about the “super size” meals or the “all you can eat” buffets.
- Our bodies tell us most of the time when we have had enough. Teach children that it is okay to stop eating when they are full. Watch their portion sizes according to their age and don’t expect them to eat the same amount of food you would eat, because their bodies do not need the same amount.
- Remember, moderation is the key and good choices are something we need to teach our children by example.
Communities Are Helping
Around the country, communities are creating programs to help combat the epidemic of childhood obesity, many based on the results of an expert committee report on the subject. In Cabarrus County, NC, for example, Children WIN – Wellness Initiative Network, is a coalition of healthcare, preschool age health, school age health, church, local government and business representatives that aims to decrease the prevalence of overweight children and improve the health of all the county’s children. They have adopted a successful national messaging program known as 5-2-1-0 as a simple way to remember what we are striving for on a daily basis for our children and for ourselves:
5-2-1-0
5 – Have at least 5 servings of fruits and vegetables per day
2 – Limit recreational screen time (not counting school time) to no more than 2 hours per day
1 – Strive for one hour of physical activity per day (this could be dancing with your children or jumping around being silly)
0 – Zero sugar sweetened beverages, with an emphasis on drinking water and low fat milk. (Meaning no sodas/no sweetened iced tea.)
When we all work together to inform families and guide children in making healthy choices, we can make improvements in children’s health by reducing the incidence of overweight and obesity.
Jomari Torres, M.D., is Research Assistant Professor, Department of Nutrition, UNC Chapel Hill and Human Research Core Medical Director at the UNC Nutrition Research Institute in Kannapolis, NC. She welcomes inquiries about childhood obesity. Jomari_torres@unc.edu